“My daughter, a RN, and I have been treated by Dr Leary for everything from varicose veins to brow furrows, over a period of many years. We have the highest regard for Dr Leary’s professionalism and results. The offices have been well managed and our waits have been minimal. Appointments have actually been a pleasant experience.”
- C. Shaw
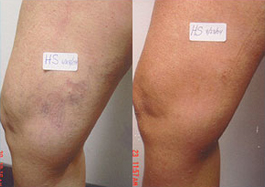
“I have just completed my 2nd session of sclerotherapy & have already seen results even after my 1st session . I have been to several other Doctors over the years & have never had such a positive experience with results & a pain-free outcome . I feel very fortunate to have found Dr Leary.”
- D.G.
“Dr. Leary took a lot of time with me and was very detailed. He walked me through what causes the symptoms. He went through the different options to fix to the problem and suggested the best solution for me. He did a great job of managing my expectations. He has extraordinary bedside manner. My legs are now 100%. I don’t have to worry about the throbbing feeling or the pain associated with varicose veins. Aesthetically, my legs look great.”
- Eric S.
I have to tell you again that I’m absolutely thrilled with the work that Dr. Leary has done – I’ve had 4-5 sclerotherapy appointments with him and it’s been terrific. The difference is amazing – I’m definitely ready for summer! When I was in this morning I told him that I wish I’d done this ages ago. He is phenomenal and his work is wonderful. The entire team is so warm, friendly and accommodating – I’ve already told friends and am encouraging them to call you so I hope they do! I’ll see you on the 27th!
- Erika
Hello,
I guess that I don’t know where to start without boring you, so I’ll be as brief as possible. I think of all the years that I have worn long skirts or pants; of going to the beach and not taking my sarong off to hide my legs. I have envied women wearing short skirts and not wearing black stockings to hide their legs as I often did. And I have been doing all of the above, since I was 23 years old.
When I heard your commercial on Air America Radio, I was curious, and looked California Vein Specialists on-line. I read Dr. Michael Leary’s bio, was most impressed, and made an appointment for my exam.
Your staff immediately made me feels welcome. Dr. Leary gave me an ultra sound exam on my legs, explained what procedures would be done, and made me feel very much at ease.
The following procedures over the past few months have proved so successful, that my family and friends are amazed! My husband and children had never seen me without veins and are thrilled to see me wearing shorts and dresses that I would never have worn before.
I will never be able to thank you enough, for what you’ve done for me. I promise to “spread the Gospel” and become a missionary forCalifornia Vein Specialists. Maybe I can help other people to realize their dream as well, of VEIN – FREE LEGS!!!!!!!!!!!
Thank you again,
- Barbara L.
Dear Dr. Leary and Staff,
Happy New Year! I had EVLT last January 29 on my left leg. I have been more active this past year, attending “boot camps” and walking/running a lot. I have no more lumps, and the purple discoloration is miniscule!
YAY!!! As soon as I have time, I am coming in for spider vein treatment on my face and right leg. Thank you, and the best to you all in 2009!
- Christina W.
I am so pleased with how my legs look and feel! Over the past 20 years, I have had various types of treatments in several cities for my varicose veins, and Dr. Leary is the best. Never have I seen such noticeable improvement in such little time. Dr. Leary and your entire staff are caring and professional. You were recommended to me, and now I see why. I will definitely be recommending you to others!
- Pat B.
I experienced leg cramps. I came in to see Dr. Leary and got treated right away. I was totally satisfied with Dr. Leary’s procedure and the whole experience.
- Actual Patient
I had large, bulbous veins on the front of the my legs where they were very noticeable. I like to wear shorts and I’m very athletic. I run, I go to the gym and the vein was right in front where I would always see it.
I liked the idea of not having surgery and just having a procedure where it could be injected. That was a big plus for me. I exercise everyday and I had no downtime. I had to wear a compression stocking but was able to exercise right away. I am very pleased with the results. I wear shorts and dresses and no longer feel self-conscious.
- Sharon H.